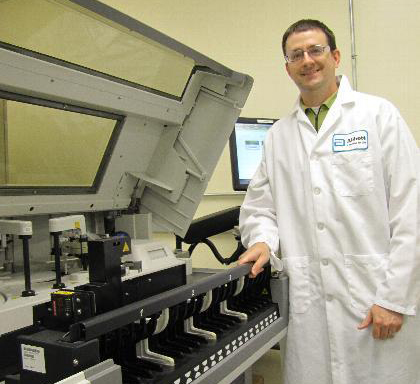
IRVING, TX – Abbott Laboratories is at the forefront of efforts to develop testing for coronavirus, producing two tests to date that identify the presence of the virus that causes COVID-19. Alfred University alumnus James Hart has been closely involved in a third test, launched last week, which can detect whether a person has been previously infected.
The Sigma Alpha Mu brother, who grew up in Wilcox, PA—about 30 miles south of Bradford, PA, and a two-hour drive from Alfred—received a bachelor’s degree in chemistry from Alfred University in 2001. He has been with Abbott Laboratories for nearly a decade, serving since last July as medical director of Abbott’s Diagnostics Division in Irving, TX.
“In diagnostics, we develop a variety of tests that diagnose disease and determine how healthy, or unhealthy, a person is,” said Hart. As medical director, he is “charged with providing input from a medical doctor’s perspective and a laboratory scientist’s perspective. My primary focus is ensuring that the tests we produce provide safe, accurate results to help patients live their best lives.”
Abbott’s first coronavirus test, the RealTime COVID-19 test, received emergency authorization from the federal Food and Drug Administration on March 18. The test runs on Abbott’s m2000 instrument, a larger machine typically found in a hospital or medical laboratory setting. Abbott initially deployed more than 150,000 of the tests to medical facilities in 18 states, including New York, and has since ramped up weekly production to one million tests.
The ID-NOW COVID-19 test, which received FDA emergency authorization on March 25, runs on Abbott’s ID-NOW platform, a hand-held unit that can return a positive result in as little as five minutes and a negative result in as few as 13 minutes. Abbott is working to increase production of the ID-NOW tests to five million per month. The portability of the ID-NOW unit is key, as it allows testing to be brought to the front lines of the battle against coronavirus.
Hart has been closely involved in Abbott’s most recent test, launched last Wednesday, April 15, which uses serology to detect the antibodies produced to fight off infection by the virus.
“With this new test, we use a normal blood draw to obtain a sample instead of the nasal swabs that are needed to run the viral detection tests. This test looks for the presence of coronavirus-specific antibodies circulating in the bloodstream,” Hart explained. The test runs on Abbott’s ARCHITECT instruments, each of which can run up to 100-200 tests per hour.
This serology test detects the IgG class of antibodies, which are proteins the body produces in the later stages of an infection that may remain in the body for months or even years after a person has recovered. The tests are key because not all people infected with the coronavirus show symptoms of COVID-19; by detecting these antibodies, the tests can identify if those people have been exposed to the virus. With that knowledge, scientists can better understand how long antibodies stay in the body and how much immunity they provide, and public health officials will have a better grasp of how widespread the outbreak actually is. Abbott expects to distribute four million of the antibody tests throughout the United States before the end of April.
All three tests run on existing instrumentation that is already widely used to test for a variety of infectious diseases and other medical conditions, Hart explained. “The advantage is that, in many locations, hospitals won’t need to learn how to operate a new device to use our tests. We just need to send them the new reagents to run these tests on the instruments that are already in their labs.”
The effectiveness and significance of the new testing procedures will be better understood in the weeks and months ahead, Hart noted.
“We have to start running a lot of tests throughout the world, over time, to fully understand what the results mean,” he said. The hope is that people who have become infected with the virus and recovered will develop a long-lasting immunity, similar to what occurs with chicken pox. “Hopefully, we will get good news. This serology test represents a very important next step in understanding and containing this disease.”
Hart matriculated at Alfred University in 1997 after what he describes as a typical college search. “Alfred was on the short list for me—a small school, not far from home. As a National Merit Scholar, I was fortunate to qualify for a full scholarship.”
At Alfred, Hart played on the varsity tennis team during his first two years and was a member and president of Sigma Alpha Mu fraternity.
“I felt right at home in the Alfred community during my college years,” he said. “To this day I’m extremely grateful for the advice and friendship of my faculty advisors— Dr. Wesley Bentz, Dr. James Curl, and Dr. Garrett McGowan.”
Hart had originally aspired to practice medicine. After graduating from Alfred, he joined the National Institutes of Health-funded Medical Scientist Training Program at the University of Rochester, and soon his career interests shifted toward medical research. In 2010, after earning doctoral degrees in medicine and biophysical chemistry from the University of Rochester, he began his career at Abbott Laboratories.
He has held several positions in Abbott’s Diagnostics Division, including systems engineer, engineering manager, and systems development manager. He joined Abbott’s Medical Affairs organization in 2017, serving as associate medical director until his promotion to medical director last July.
Other diagnostic testing projects Hart has been involved with include the development of Alinity, Abbott’s family of systems designed to simplify diagnostics across key laboratory disciplines. The Diagnostics Division at Abbott has also been at the forefront of developing tests that quickly and effectively diagnose heart attacks and other cardiac-related events.
“Advancing medical science in this field has been very exciting. If we are able to design better tests, we can improve outcomes for many patients,” Hart said. “For example, we can use information from newer cardiac markers to more accurately predict the risk of someone having a heart attack in the near future. It moves us more toward prevention rather than emergency response.”
The significance of the work being done to combat the COVID-19 pandemic can’t be overstated, and Hart is well aware that the world is looking to the scientific community with a hopeful eye. “This has brought our industry into the spotlight. My older colleagues say the most recent parallel to this is the HIV epidemic of the 1980s. This has been a very busy time for us.”
How does Hart feel being so closely involved in such important research?
“There are two competing feelings,” he says. “One, it’s pretty humbling to be reminded on a daily basis that our work is this important. We are usually behind the scenes, but now we’re front and center. Second, it is a validation of my career choice. I entered medical school with the idea of becoming a practicing medical doctor but was drawn toward a career in research. Now I’m in this lab in Texas and my work could literally impact the lives of millions of people. It is potentially world changing. How cool is that?”
Hart lives in the Dallas suburb of Grapevine, TX, with his wife and fellow Alfred University alumnus, Jennifer (Burke) Hart, and their two daughters, Sarah, who turns 8 in May, and Samantha, 6.
Jennifer, who earned a bachelor’s degree in psychology from Alfred in 2002, taught elementary school classes for several years in New York and Texas before staying home to raise Sarah and Samantha. She was recently working with Mental Health America of Greater Dallas, a non-profit organization that promotes and advocates for mental health awareness in the Dallas area, but has temporarily stepped back from that role due to the COVID-19 crisis.